Imagine waking up every morning feeling like you’ve run a marathon in your sleep. Your limbs are heavy, your brain is foggy, and the thought of facing the day ahead seems as daunting as climbing Everest. Welcome to the world of Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME).
If this sounds familiar, you’re not alone. An estimated 17 to 24 million people worldwide are wrestling with CFS/ME, according to the Institute of Medicine. That’s a lot of people feeling like they’re wading through molasses just to get through the day.
But here’s the thing – while CFS/ME is a serious condition, it doesn’t have to be a life sentence. With the right strategies and support, many people with CFS/ME have found ways to manage their symptoms and improve their quality of life.
Understanding CFS/ME
Before we dive into strategies, let’s clear the fog around what CFS/ME actually is. Despite what some misinformed folks might say, CFS/ME is not “all in your head” or “just being lazy.” It’s a real, physiological condition recognized by major health organizations worldwide.
The hallmark of CFS/ME is profound fatigue that doesn’t improve with rest and worsens with physical or mental activity. But it’s not just about being tired. CFS/ME can also involve:
- Post-exertional malaise (PEM): A crash of symptoms after even minor exertion
- Cognitive difficulties (often called “brain fog”)
- Unrefreshing sleep
- Orthostatic intolerance (dizziness or fainting when standing up)
- Pain (muscle pain, joint pain, headaches)
- Sensitivities to light, sound, or chemicals
Dr. Nancy Klimas, a leading CFS/ME researcher, describes it as “a flu that never goes away.”
The CFS/ME Puzzle
One of the frustrating aspects of CFS/ME is that its exact cause remains unknown. However, researchers have identified several factors that may contribute:
- Viral infections: Many people report that their CFS/ME started after a viral illness. The Epstein-Barr virus, human herpesvirus 6, and enteroviruses have all been implicated.
- Immune system dysfunction: Studies have found abnormalities in the immune systems of people with CFS/ME, suggesting an autoimmune component.
- Hormonal imbalances: Some research points to abnormalities in the hypothalamic-pituitary-adrenal (HPA) axis, which regulates stress response and many bodily processes.
- Mitochondrial dysfunction: The powerhouses of our cells may not be working efficiently in CFS/ME.
- Genetic predisposition: While not a direct cause, certain genes may make some people more susceptible to developing CFS/ME.
Understanding these potential factors can help guide treatment approaches. As Dr. Anthony Komaroff, a Harvard physician and CFS/ME expert, puts it: “CFS/ME is like a thousand-piece jigsaw puzzle. We’re slowly putting the pieces together, but we don’t have the full picture yet.”
Strategies for Managing Symptoms
While there’s no one-size-fits-all treatment for CFS/ME, there are numerous strategies that can help manage symptoms and improve quality of life. Remember, what works for one person may not work for another, so it’s all about finding your unique combination.
1. Pacing
Pacing is perhaps the most crucial strategy for managing CFS/ME. It involves balancing activity and rest to avoid post-exertional malaise (PEM).
Try this:
- Keep an activity diary to identify your energy patterns
- Use a heart rate monitor to stay within your anaerobic threshold
- Practice the “spoon theory” – allocating your limited energy (spoons) wisely throughout the day
A study published in the Journal of Health Psychology found that pacing was associated with improved physical functioning in people with CFS/ME.
2. Sleep Hygiene
While people with CFS/ME often experience unrefreshing sleep, improving sleep hygiene can still make a significant difference.
Here’s how to optimize your sleep:
- Stick to a consistent sleep schedule
- Create a relaxing bedtime routine
- Make your bedroom a sleep sanctuary – dark, quiet, and cool
- Avoid screens for at least an hour before bed
3. Nutrition: Fueling Your Body Right
While there’s no specific “CFS diet,” eating a balanced, nutrient-rich diet can help support your body’s energy production.
Consider:
- Eating smaller, more frequent meals to maintain steady energy levels
- Focusing on whole foods rich in vitamins and minerals
- Staying hydrated – dehydration can exacerbate fatigue
- Considering supplements like B-vitamins, magnesium, and Coenzyme Q10 (but always consult with your healthcare provider first)
A study in the journal Nutritional Neuroscience found that a low sugar, low yeast diet improved symptoms in some CFS/ME patients.
4. Gentle Movement
Exercise can be a double-edged sword for people with CFS/ME. While complete inactivity can lead to deconditioning, overexertion can trigger PEM. The key is finding your personal “sweet spot.”
Try this:
- Start with very gentle activities like stretching or tai chi
- Gradually increase duration and intensity as tolerated
- Always listen to your body and stop before you feel tired
Research published in the Physiotherapy Theory and Practice journal found that individualized exercise programs can improve functioning in CFS/ME patients when done carefully.
5. Stress Management
Stress can significantly worsen CFS symptoms, so learning to manage it is crucial:
- Practice mindfulness meditation
- Try deep breathing exercises
- Consider gentle yoga or qigong
A study in the Annals of Internal Medicine found that mindfulness training reduced fatigue severity in CFS/ME patients.
6. Cognitive Behavioral Therapy (CBT)
While CBT doesn’t cure CFS/ME, it can help you manage the condition more effectively by changing how you think about and respond to your symptoms.
CBT can help you:
- Develop coping strategies
- Improve sleep
- Manage activity levels
- Deal with the emotional impact of CFS/ME
A large-scale study published in The Lancet found that CBT, when used alongside specialist medical care, moderately improved outcomes for CFS/ME patients.
Conclusion: Navigating Life with CFS/ME
Living with CFS/ME is undoubtedly challenging, but it doesn’t mean life is over. Many people with CFS/ME have found ways to adapt and even thrive despite their condition.
Remember:
- Be patient with yourself. Healing takes time.
- Celebrate small victories. Getting out of bed can be a triumph on bad days.
- Connect with others. Support groups can provide invaluable understanding and tips.
- Stay hopeful. Research is ongoing, and new treatments are on the horizon.
As Laura Hillenbrand, author of “Seabiscuit” and a CFS/ME sufferer herself, beautifully puts it: “When you’re struggling with something, look at all the people around you and realize that every single person you see is struggling with something, and to them, it’s just as hard as what you’re going through.”
You’re not alone in this journey. While CFS/ME may have changed your life, it doesn’t define you. You are so much more than your illness. Keep pushing forward, and remember—you’re not alone in this fight.
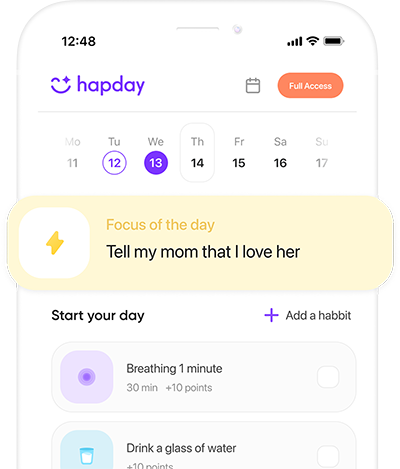
Manage CFS/ME symptoms with Hapday, Your Wellbeing Assistant
Join the millions of people using Hapday. Improve overall wellness & sleep.